- After breast cancer, cervical cancer is the second leading cause of cancer deaths
- Western region (followed by the South) had most prominence of HPV infection, which causes cervical cancer
New Delhi, January 31st, 2018 : A retrospective analysis of HPV (Human Papillomavirus) testing in Cervical Cancer Screening by SRL Diagnostics – the leading diagnostics chain in India – has revealed that samples received from women from 16 – 30 years (14%) age group had the highest percentage of positive cases of high risk HPV, and hence a chance of developing cervical cancer. It was followed by the percentage in women from the 61-85 years (8.39%) age group. More than 3,000 women were tested pan-India between 2013 and 2017 for High Risk HPV infection by using the global standard method – Hybrid Capture II. Overall, 8.04% women showed high-risk HPV infection. More women from western India (about 10.23%) had high risk HPV infection than those from any other zone, closely followed by women from the South (about 9.78%) zone.
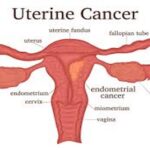
The tests utilized in the screening for cervical cancer are – Conventional (Pap) test and Liquid-based Cytology (LBC), Visual Inspection with Acetic Acid (VIA) and HPV testing for high-risk HPV types. In this analysis by SRL test data of HPV by Hybrid Capture 2 were used.
India accounts for nearly one-third of all global cervical cancer deaths, with approximately 1, 32,000 new cases being diagnosed and 74,000 deaths occurring annually. After breast cancer, cervical cancer is the second leading cause of cancer deaths, accounting for 17% of all cancer mortalities among women between 30 and 69 years, where the median age is 38 years. India ranks highest in the age-standardized incidence of cervical cancer in South Asia at 22 per 100,000 population.
Almost 100% of cervical cancers are caused by long-term (over a decade), persistent HPV infections. Among 100 different HPV types, 8 most common high-risk HPV types: 16, 18, 45, 33, 31, 52, 58, and 35 account for 91% of all cases of cervical cancer. HPV 16, 18, and 45 are known to occur in 75% of the most common type of cervical cancer (squamous cell) and in 94% of adenocarcinomas (the second most common form). Considering its role in cervical cancer, HPV testing has become an essential part of current clinical practice mainly for the management of cervical cancer and precancerous lesions.
Studies in India indicate about 5% of women in the general population are estimated to harbor cervical HPV-16/18 infection at a given time. Elaborating on this Dr B.R Das, Advisor and Mentor – R&D and Molecular Pathology, SRL Diagnostics said, “Though most of HPV infections clear up on their own and most pre-cancerous lesions resolve spontaneously, persistence of such high-risk HPV infection has 100 fold risk of high-grade cervical cancer. Therefore, main goal of cervical cancer screening should be to detect and treat pre-cancer before cancer develops”.
PAP test is the most commonly used screening test, however PAP test is much more likely to miss precancerous cervical disease than HPV testing. Available data indicates HPV testing is more sensitive for detecting localized infection and marginally less sensitive for distant infection. Owing to these limitations, co-testing in women between 30 and 65 years is the preferred screening strategy recommended by most of the global medical associations. It is recommended to be performed every 5 years. Nevertheless experts believe that screening benefit of co-testing is largely driven by HPV testing and not cytology.
In India, in spite of alarmingly high figures, there is no nationwide government-sponsored screening program. Due to affordability issues and lack of awareness, reflex testing is more popular particularly in suspected/high-risk cases. Stressing the importance of right screening strategy, Dr. Das added “That getting checked for cervical cancer isn’t one size fit all, but most importantly if it is detected early the five year survival rate goes up to 91%. Research indicates that approximately 80% of women diagnosed with cervical cancer have never been screened or have not had regular Pap smears. The main choice moving forward is between reflex testing, co-testing or HPV testing alone. There is no cure for HPV. If detected early, problems associated with the virus (such as warts) can be treated. HPV screening aids in screening of cervical cancer in the early stages and early detection is key for stopping cervical cancer”.