PIB Webinar Doctors throw light on Mucormycosis and its prevention
“If you get COVID-19 after vaccination, it will be mild in vast majority of cases”
New Delhi, June 3, 2021
The cases of Mucormycosis we are witnessing are a tiny fraction of COVID-19 cases, informed Gastroenterologist Dr. Rajeev Jayadevan during a webinar on ‘Mucormycosis and Dental Health in relation to COVID-19’, organized by the Press Information Bureau today. The other expert panelist in the webinar was Prosthodontist Dr. Neeta Rana. The doctors’ advice and knowledge imparted in the webinar are presented in form of key points below.
What makes people prone to Mucormycosis?
Explaining what makes COVID-19 patients prone to mucormycosis, Dr. Jayadevan said, “Having COVID-19 in the background of diabetes and steroid use, is a classic setting for triple immune suppression. COVID-19 affects many segments of our body, including our immune system”. Stating that there is a link between diabetes and mucormycosis, the doctor informed, ” Many people in our country have diabetes. Given this and our population, the number of people who fall sick is higher than in any other country. So, it is understandable that some of them will catch Mucormycosis.”
Dr. Jayadevan, who has written several articles for doctors, policy makers and the general public during the pandemic, opined, “The way I see it, a tiny proportion of the large number of people getting infected with COVID-19 are getting infected with mucormycosis, so this proportion becomes a large number”.
The doctor further explained: “Mucormycosis cases have been seen in people with decreased immunity, predominantly either due to diabetes or after some organ transplant. In the last month or two, we have seen a rise in mucormycosis in those without these conditions. It is a new development. But we need studies need to confirm reasons for increased cases in those without traditional risk factors.”
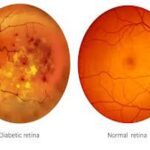
Diabetes and Mucormycosis
Dr. Jayadevan says, “For diabetic patients, when the blood glucose of sugars cannot be controlled, the immune system is not able to work properly. In case of severe diabetes, the function of pathogen-fighting cells like neutrophils gets impaired. Factors such as this make us prone to contracting mucormycosis. High sugar level in itself is conducive to fungal growth. Fungus loves sugar, it loves trace metals like zinc, it also grows on dead tissue and until the body repairs the dead tissue, fungus may grow on it”.
In the next stage, “The fungus invades our blood cells, our tissues don’t get oxygen supply and die, and when the tissues die, they become black in colour. This is the reason why the name black fungus is used for Mucormycosis”, explained the gastroenterlogist in simple terms for the benefit of lay people.
Dental Health and Mucormycosis
The dental expert Dr. Neeta Rana explains, “There is definitely a link between good dental health and COVID-19 infection. When teeth, gums and palette are maintained well, naturally present microorganisms will function well and viral infection is less likely to occur. If wound after tooth-extraction is not maintained well, if good oral hygiene is not observed, then we increase chances of catching Mucormycosis”.
Brushing of teeth, flossing, mouth-washing and rinsing will also help in maintaining good dental health, advised Dr. Neeta.
Vaccination and Mucormycosis
Dr. Jayadevan says, “If you get COVID-19 after vaccination, it will be mild in vast majority of cases”. The doctor further suggested that medicines are not necessary in mild cases of COVID. Hence, in cases of mild COVID-19, the chance of catching steroid-related mucormycosis will be low, opined the doctor. “But if instead of letting the mild COVID case cure by itself, if the person starts self-medication, taking medicines which are not required, it may set the stage for a fungal infection that would have never happened in the first place”, he cautioned.
Post-COVID and Mucormycosis
Dr. Jayadevan says, “Effects of immuno-suppression and COVID-19 treatment will remain in body for some time, just like we see ripples in a river, long after a boat goes through the river”. Hence, his advice is to ‘Remain Vigilant for a few weeks after recovering and not do anything adventurous or experimental with your body’. In the context of immuno-suppression causing patients to become prone to Mucormycosis, Dr. Jayadevan informs, “So many studies have conclusively shown that good healthy bacteria living in our body improve our body’s defence against invading bad bacteria. So, prolonged and unnecessary use of antibiotics is a strong risk factor for fungal and bacterial infections”. In this connection, Dr. Jayadevan reflected that vast majority of people in our country engage in some form of self-treatment. The doctor strongly discouraged this practice. His advice in this regard: “Just follow the basic instructions given by the doctor you are in touch with and stay away from unnecessary medicines”.
Whether Mucormycosis infection comes from surroundings?
Dra. Jayadevan says, “Fungus is there all around us. Do not be excessively scared of venturing out due to fear of catching fungal infection. Fungi have existed for centuries, and Mucormycosis is a rare infection, occurring in very few cases”.
Dental Care in times of a pandemic
Dr. Neeta advises, “Be in touch with your dental doctor, teleconsultation will help in many cases. If guidelines are followed at dental clinics, there should not be reason for fear of catching any infection, but don’t be overzealous too. Follow doctor’s advice about physical visit to a dental clinic”.
How long vaccines can provide immunity against COVID-19?
Dr. Jayadevan explains, “When we encounter repeat infection or infection after vaccination, memory cells introduced in previous infection will swing into action immediately. Studies show that memory cells last at least an year”. Explaining the function of vaccines, the doctor said, “What vaccines do predominantly is to prevent severe disease or death on getting infected; a good number of scientists believe that immunity from vaccination is reasonably long-lasting, likely to protect us for many years”.
Advice for those exposed to COVID-19
Dr. Jayadevan says, “Never take it lightly. There is no need to panic. But, after 5-6 days, if your symptoms are worsening, if you are getting tired, short of breath, unable to eat, chest pain or simply not feeling well, then go to a hospital and see a doctor. Alternatively, you can do teleconsultation with a doctor also”.
healthysoch